The sooner any cancer can be correctly diagnosed, the better chances of a curative scenario for the person concerned. However, some cancers are in the ‘difficult to diagnose’ category. Certain types of Neuroendocrine Tumours (NETs) are in this difficult to diagnose category due to the vague symptoms which may be mistaken for other diseases and routine illnesses. However, in many cases which don’t seem to make the statistics, it can be incredibly quiet leading to incidental diagnosis including at an advanced stage. It’s sneaky!
Some of the most common misdiagnoses appear to be Irritable Bowel Syndrome (IBS), asthma, or menopause. Patients complain of abdominal pain, wheezing, shortness of breath, diarrhea, flushing, palpitations and a whole host of other minor issues. There are even extreme cases where patients have been told they may have a mental illness following constant visits to their local doctors. These cases can lead to months or in extreme cases, even years of delay from the onset of symptoms.
NETs are dangerous despite the normally indolent course but they have a propensity to metastasize meaning that the chance of a curative scenario is vastly decreased for many. It can kill if left untreated.
Neuroendocrine tumors (NETs) are highly vascularized, but the process of proliferation and maturation of vascular structures during tumor development and progression has remained unknown.
A Gallium 68-DOTA PET CT is a test used to check the body for the presence of neuroendocrine tumor cells. This test is done in the Nuclear Medicine Department. Improvements in the usage of more advanced diagnostic tools are needed to help achieve early detection of NETs. This advanced and more precise diagnostic tool has significantly lower usage vs more common diagnostic tools globally and locally. We need to spread the word among the medical community and make more awareness of NETs!
“Patients present in an almost surrealistic manner – a mix of tumor- related symptoms and signs, with bizarre and sometimes grotesque endocrine syndromes”
There is no cure available for neuroendocrine tumors available yet but as usual, there is treatment. The prognosis of the patient can be decided on the basis of stage and grade of cancer and certain other factors like age, the general condition of the patient. All these factors are looked at collectively to determine the prognosis of the tumor.
Brain metastases are rarely reported in patients with neuroendocrine carcinoma (NEC) of non-lung origin and neuroendocrine tumors (NETs) of the gastro-entero-pancreatic or bronchopulmonary system. Symptomatic brain metastases are associated with a dismal prognosis, so early detection and treatment could be advisable.
The incidence of brain metastases for neuroendocrine tumors (NET) is reportedly 1.5~5%, and the origin is usually pulmonary.
If brain metastases are present, lymph node metastases are found in 75% and liver metastases are found in 50% of these patients. Especially for functional NETs, because patients have specific symptoms when the tumor size is small. Somatostatin receptor scintigraphy (SRS) is useful to detect the primary focus.
NETs are well known for being heterogeneous. They can arise from a variety of different organs; can be benign or malignant; are well, moderately, or poorly differentiated, as in grade; have variable metastatic potential; and are either functional or nonfunctional (i.e., produce hormones and symptoms or do not) . Symptoms can markedly reduce quality of life and are an important consideration for therapy. NETs have a low incidence but a high prevalence given the lower mortality associated with these tumors.
Brain metastases are the most common intracranial neoplasm in adults. They often originate from lung cancer, breast cancer, or melanoma, but also other malignancies like renal cancer, colorectal cancer, and ovarian cancer are increasingly associated with brain metastases.
"Over the past two decades, SSTR-targeted imaging using radiolabeled somatostatin agonists followed by PRRT has been remarkably successful in managing neuroendocrine tumors," said Jingjing Zhang, MD, Ph.D., assistant professor in the Department of Diagnostic Radiology at the Yong Loo Lin School of Medicine at the National University of Singapore in Singapore. "However, potent SSTR antagonists—which only poorly internalize into tumor cells if at all—have surprisingly been shown to be even superior to agonists for such purposes."
To further investigate the role antagonists can play in treating neuroendocrine tumours researchers developed a study to determine the safety, bio distribution and efficiency of a new type of SSTR antagonist, 177Lu-DOTA-LM3. Fifty-one patients with progressive, heavily pretreated neuroendocrine neoplasms underwent PRRT with 177Lu-DOTA-LM3. Treatment-related adverse events were graded for all participants, and dosimetry was performed for patients.
177Lu-DOTA-LM3 was administered without severe adverse effects and was well tolerated by most patients.
Of note, the uptake and dosimetry( ”Dosimetry” refers to the science by which radiation dose is determined by measurement, calculation, or a combination of measurement and calculation. The technical name for radiation dose is “absorbed dose”; it is the amount of radiation energy that is deposited in tissue divided by the mass of the tissue. )of the antagonist 177Lu-DOTA-LM3 were compared with those of the commonly used SSTR agonist 177Lu-DOTATOC in patients undergoing treatment on the same dosimetry protocol. 177Lu-DOTA-LM3 demonstrated higher uptake and a longer effective half-life in tumor lesions, resulting in higher tumor radiation doses than for agonist 177Lu-DOTATOC.
The neuroendocrine system comprises a complex architecture of cells that are capable of producing NETs throughout the body. While NETs are known to develop throughout the gastrointestinal and respiratory tracts, there are only a few reports to suggest NETs originating primarily from the brain. NETs can be well-differentiated or poorly differentiated, and in the high grade poorly differentiated types, they can be large cell or small cell variants. The incidence of NETs has been prominently increasing over the past two decades. This is believed to be secondary to increased detection rates. Generally, the majority of NET metastases occur in the liver, lungs, and bone.Involvement of other sites is much rarer. NETs are considered to be the origin of brain metastases in 1.5-5% of all patients that.have brain metastases. If brain metastases are present, lymph node metastases are found in 75%, and.liver metastases are found in 50% of these patients. Primary unknown NET represents just 13% of these tumours.
NETs is secondary to systemic disease progression, the prognosis may be substantially different from metastatic brain NETs.Primary brain NETs appear to be more similar to non-metastaticNETs in which the ten-year overall survival rate is 47%
"These encouraging findings demonstrate the feasibility and superiority of SSTR antagonist 177Lu-DOTA-LM3 as compared to SSTR agonists. Furthermore, antagonist PRRT can be performed under concurrent treatment with somatostatin analogue without the need for interrupting these medications. This is especially important for patients suffering from carcinoid syndrome or even carcinoid crisis,". "The results are very encouraging for theranostic applications of SSTR antagonists to further improve outcomes in patients with neuroendocrine neoplasms in the future."
PRRT
Peptide Receptor Radionuclide Therapy (PRRT) is a highly targeted and effective form of radiopharmaceutical therapy (RPT) with minimal side effects for treating NETs with an abundance (or overexpression of somatostatin receptors.
PRRT is an option for patients:
- Who have advanced (metastatic) and/or progressive (e.g. to SSA) neuroendocrine tumors positive on somatostatin receptor imaging (e.g. 68Ga-DOTATATE/NETSPOT or 64Cu Dotatate/Detecnet) which are radioactive tracers used with PET/CT or PET/MR machines.
- Who are not candidates for surgery
- Whose symptoms do not respond to other medical therapies
Benefits of PRRT include symptom relief, slowing tumor progression and improving overall survival.
The most common protocol includes a series of four PRRT treatments with 177Lu-DOTATATE spaced approximately 8 weeks apart. Local protocols may vary. This therapy may be done as an outpatient procedure or may require a hospital stay of a few days. In the United States, this treatment is performed as a half or full-day outpatient procedure and only in rare cases, a patient may need to stay overnight at the hospital.
Each PRRT session begins with anti-nausea pre-medications, followed by an amino acid solution. The amino acid solution is delivered intravenously to protect the patient’s kidneys from the effects of the treatment. The radioactive drug is then injected into the patient, which generally takes about 30 minutes, followed by administration of additional amino acid solution. In total, the treatment session lasts approximately four to five hours.
Post-treatment 177Lu scans may be taken during and following the treatment process to see where the injected radioactive drug has traveled in the body, although this scan is not required as part of the FDA label for treatment.
What are the advantages of PRRT?
PRRT and other molecular therapies offer more personalized cancer treatment. PRRT is targeted therapy because these radioactive drugs are highly selective in their ability to specifically reach and damage neuroendocrine tumor cells, while limiting radiation exposure to healthy tissue. As a result, PRRT is generally well tolerated.
PRRT is a treatment option that is highly effective in controlling advanced, metastatic or inoperable, progressive neuroendocrine tumors. PRRT is rarely curative but has been shown to help relieve symptoms, shrink tumors, and slow the progression of the disease.
PRRT with 177Lu-DOTATATE was FDA approved in 2018 for the treatment of gastroenteropancreatic neuroendocrine tumors. There are ongoing clinical trials featuring other radiopharmaceuticals, isotopes, peptides and combinations with other therapy.
What conditions are treated with PRRT?
PRRT is used to treat NETs,
Who have advanced (metastatic) and/or progressive (e.g. to SSA) neuroendocrine tumors positive on somatostatin receptor imaging (e.g. 68Ga-DOTATATE/NETSPOT or 64Cu Dotatate/Detecnet) which are radioactive tracers used with PET/CT or PET/MR machines.
Who are not candidates for surgery
Whose symptoms do not respond to other medical therapies.
Benefits of PRRT include symptom relief, slowing tumor progression and improving overall survival.
The administration of the PRRT itself is well tolerated, but patients may experience nausea and vomiting as a result of the amino acid solution given for kidney protection, especially with some types of amino acid solutions. This is managed with anti-nausea medication or slowing down the administration of the amino acids. Long-term side effects can include a suppression of blood cell counts, which is mild to moderate in the majority of cases. Delayed side effects, such as permanent kidney injury, or the appearance of secondary blood disorders (called myelodysplastic syndrome), are rare. Overall, the treatment is well tolerated by most patients.
Home Care
The medical facility will provide with all instructions for special care to be taken following treatment. Because small amounts of radiation temporarily remain in the body, patients need to follow the radiation safety protocol provided by your facility. This may include staying a safe distance from others for several days and careful hygiene following PRRT therapy. Because the radioactive drug is removed from the body mainly through the urine and feces, it is important to maintain good bathroom hygiene during this period.
Side Effects
The administration of the PRRT itself is well tolerated, but patients may experience nausea and vomiting as a result of the amino acid solution given for kidney protection, especially with some types of amino acid solutions. This is managed with anti-nausea medication or slowing down the administration of the amino acids. Long-term side effects can include a suppression of blood cell counts, which is mild to moderate in the majority of cases. Delayed side effects, such as permanent kidney injury, or the appearance of secondary blood disorders (called myelodysplastic syndrome), are rare. Overall, the treatment is well tolerated by most patients.
To note:
Neuroendocrine Hormonal Crisis
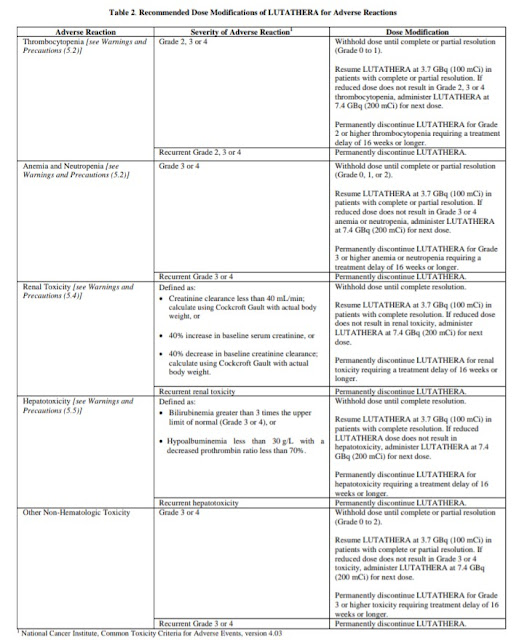
Neuroendocrine hormonal crises, manifesting with flushing, diarrhea, bronchospasm and hypotension, occurred in 1% of patients and typically occurred during or within 24 hours following the initial LUTATHERA dose. Two (<1%) patients were reported to have hypercalcemia.
Monitor patients for flushing, diarrhea, hypotension, bronchoconstriction or other signs and symptoms of tumor-related hormonal release.
Administer intravenous somatostatin analogs, fluids, corticosteroids, and electrolytes as indicated.
#LetsTalkAboutNETs #neuroendocrinecancer
My First PRRT
Next PRRT
Dosimetry scan
On a lot of medicines
- Levipil- 1gm bd
- Revotril-0.25 bd
- Nexito-5mg morning
- Sirolumus 1mg od
- MyCept 250od
- Embetta xr 50
- Dytor 10mg morning
- Pan BD
- Primolut N BD
- Eltroxin 150 morning
- Clobazam 10 mg at nignight
- Balcofen BD10/mg
Little problems like seizures, hiccups, diarrhoea is under control. Next PRRT is on 19 th December 2022. But positive attitude cures all. Dizziness nausea is there.