As a whole, the human nervous system operates in two modes: sympathetic, commonly known as ‘fight or flight’ when the body perceives a threat (stress), and parasympathetic, or ‘rest and digest’ mode. When the sympathetic mode is switched on, heart rate and breathing accelerate, and blood is directed toward the muscles for fast action, inhibiting digestion. In parasympathetic mode, we are relaxed and gastrointestinal secretion and motility increase.
As a whole, the human nervous system operates in two modes: sympathetic, commonly known as ‘fight or flight’ when the body perceives a threat (stress), and parasympathetic, or ‘rest and digest’ mode. When the sympathetic mode is switched on, heart rate and breathing accelerate, and blood is directed toward the muscles for fast action, inhibiting digestion.
In parasympathetic mode, we are relaxed and gastrointestinal secretion and motility increase.
The organs of digestion are served primarily by the Vagus nerve, one of the larger nerve networks in the body.
It’s divided into nerves in the submucosal layer that stimulate secretions and nerves deeper within the muscles of the gut which stimulate peristalsis. These nerves of course communicate with the brain through the central nervous system, but they are also rich in interneurons, or cross-links that enable the GI system to make most of its own decisions.
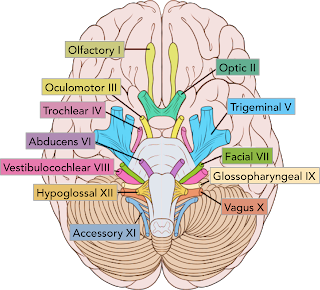
The cranial nerves associated with the swallowing process are the trigeminal (V), facial (VII), glossopharyngeal (IX), vagus (X), accessory (XI) - usually not considered - and hypoglossal (XII). It should be emphasized that the structures involved in the swallowing process are pairs, both anatomically and/or functionally, due to the dual-side innervation. Anatomically unique, the tongue, palate, pharynx, and larynx are functional pairs, each side having independent innervation.
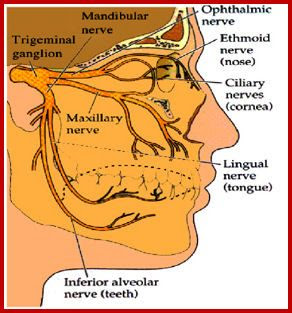
From receptors on each side of the oral cavity, the trigeminal (V), facial (VII), and glossopharyngeal (IX) nerves conduct information to the brainstem. These mixed nerves lead sensitivity (afferent pathway) and motor command (efferent pathway). The afferent pathways of the anterior two-thirds of the tongue are supplied by the lingual nerve, which associates the trigeminal (general sensibility) with the facial nerve (taste). In the posterior third of the tongue, both the general sensibility and taste are conducted by the glossopharyngeal nerve.
The trigeminal nerve (V) has three branches; upper (ophthalmic), middle (maxillary), and lower (mandibular). The upper and medium are exclusively sensitive, and the inferior, mixed. The sensitive fibers of the three branches innervate the face in transverse bands of representation. Regarding the oral cavity, the middle branch (maxillary) has sensitive responsibility for the upper arcade teeth, upper lip, cheeks, hard palate (mouth mucosa), and mucosa of the rhinopharynx. The sensitive portion of the lower branch (mandibular) is responsible for the sensitivity of the lower arcade teeth and lower mucosa of the mouth, as well as by the general sensitivity of the anterior 2/3 of the tongue.
From the trigeminal ganglion to the brainstem, all the sensory pathways will end in the posterior portion of the brainstem, over the trigeminal sensitive nucleus that occupies the medulla oblongata (spinal tract nucleus of the cranial nerve V), the pons (main sensory nucleus of the cranial nerve V) and the midbrain (midbrain nucleus of the cranial nerve V). Centrally the sensitive fibers divide into short, ascending branches that end in the main sensorial nucleus, to attend to tactile sensibility, and into long, descending branches that serve to tact, temperature, and pain, also providing collateral pathways to the spinal nucleus of the cranial nerve V.
It is believed that proprioceptive fibers from the midbrain nucleus of the trigeminal nerve in synapse with its motor nucleus located in the upper portion of the pons, would be able to integrate important chewing reflex arcs. Unless expressly desired, these arcs allow reflex modulation of chewing intensity based on bolus consistency variations, even during the voluntary bolus chewing preparation.
The motor root of the trigeminal nerve emerges from the ventral portion of the pons and runs through the mandibular root to innervate the chewing muscles, the mylohyoid, the anterior belly of the diagastric, and the tensor muscle of the palate.
The facial nerve (VII) is a mixed one, considering its motor root in association with the sensitive root given by the intermediate (Wrisberg) nerve1. The taste of the anterior two-thirds of the tongue on each side are its responsibility. From the tongue, this afferent, pre-ganglionic route follows through the lingual nerve (association of nerves V and VII), and afterward through the tympanic cord nerve (facial branch), to make synapses on the geniculate ganglion. Through the intermediate nerve, the postganglionic fibers (afferent visceral special - gustative route) synapse in the solitary tract nucleus of the medulla oblongata, associated with the general afferent visceral fibers, providing sensitive innervation to the mucosa of the nasal cavities and soft palate.
The parasympathetic efferent fibers of the facial nerve, originating from the upper salivary nucleus located on each side of the upper portion of the medulla oblongata, run through the intermediate nerve and afterward through the tympanic cord nerve to make synapses in the submandibular ganglion. Thence, through postganglionic fibers, they stimulate salivary secretion of the submandibular and sublingual glands.
The motor portion of the facial nerve has its nucleus on the ventral portion of the pons. Its fibers stimulate the skin-inserted muscles in the face, neck, and scalp, as well as the posterior belly of digastric and stylohyoid muscles.
The glossopharyngeal (IX) nerve comes out of the skull together with the vagus (X) and accessory (XI) nerves. The visceral general afferent and the visceral special afferent fibers of the glossopharyngeal nerve are associated. The visceral general afferent fibers are responsible for the general sensitivity of the oropharynx mucosa and the posterior third of the tongue, and the special visceral afferent fibers, for the taste of the posterior third of the tongue. These preganglionic fibers make synapses with the upper ganglion. The postganglionic fibers will end at the solitary tract nucleus.
The glossopharyngeal nerve’s efferent pathways come from two distinct nuclei of the medulla oblongata, the salivary inferior (parasympathetic) nucleus and ambiguous motor (special visceral efferent) nucleus. The parasympathetic fibers stimulate the salivary secretion after synapses with the optic ganglion, from which postganglionic fibers emerge to innervate the parotid gland1,29,31.
The glossopharyngeal nerve’s only motor role is with the stylopharyngeus muscle. Nevertheless, it has already been considered as motor to the superior pharyngeal constrictor muscle, whose activity had been previously attributed to the vagus nerve, responsible for the motor innervation of all pharyngeal constrictor muscles.
The vagus (X) nerve has relationships extending from the cervical region to the abdomen (transverse colon). Its sensory afference (sensory pathway) connects with the solitary tract nucleus located in the medulla oblongata. The visceral special efference (motor pathway) comes from the ambiguous nucleus in the ventral region of the medulla oblongata, and the parasympathetic fibers (visceral general efference), from the dorsal motor nucleus of the vagus.
Motor neurons that direct digestive gland activities (secretion) and smooth muscle contraction (peristalsis) Some of the neurotransmitters at work in the ENS include acetylcholine, norepinephrine, GABA, serotonin, substance P, and vasoactive intestinal peptide. We recognize some of these also as hormones, and communication chemicals important also in mood, stress, and immune response. Hormones orchestrate much of homeostasis, or the maintenance of balance in the human being. This is quite a complex feat, and it’s the balance, or relationship of hormones to one another that facilitates equilibrium. Hormones from many different glands, including the kidney, heart and organs not usually associated with the endocrine system, all function in relationship to one another, for example high levels of some feed back to reduce levels of others. That’s how something like stress can impact other hormonal functions, like a late menstrual period or even changes to one’s cycle.
There are two ways that the condition of the gut tissue impacts, and can be impacted by the condition of the rest of the body. One is reflexive action – because the GI tract arises from the same cells in the embryo as respiratory and urinary tissue, they are all linked.
Where there is tension, stagnation, weakness or hypersensitivity become generalized throughout the body. In this case, normalizing the overall tissue state will address both nervous and digestive systems, along with the rest of the body. For example stimulating sluggish digestive, liver and circulatory function will also stimulate better, quicker nerve and hormonal communication.
Because digestion is controlled by both nervous and endocrine sytems, both can impact how well our GI tract functions. It’s well known that stress is positively correlated with several GI conditions, including ulcers, irritable bowel syndrome/spastic colon and inflammatory bowel diseases including ulcerative colitis. Especially chronic stress promotes the body’s secretion of inflammatory mediators – communication chemicals that the ENS recognizes that can initiate or exacerbate inflammation. The state of the digestive organs and their function can also, conversely, affect one’s mood. For example, stagnation in the gut—gas, bloating, constipation – can lead to feelings of gloom and depression. Irritation to the intestines, from food allergens, junk foods or poorly digested food, can result in irritability of the emotions as well.
The visceral special afferent (taste) and visceral general afferent (sensibility) pathways of the vagus nerve, after synapses in a peripheral ganglion (lower or caudal), have their postganglionic fibers end at the solitary tract nucleus, similar to that observed in the intermediate portion of the facial nerve and in the glossopharyngeal one. The visceral general afferent fibers conduct impulses related to the sensitivity of the pharynx, larynx, trachea and esophagus, and the visceral special afferent route lead taste stimuli from receptors on the vallecula and from a small posterior area of the tongue next to the vallecula.
The visceral general efferent (parasympathetic) fibers of the vagus nerve originate in the vagus dorsal motor nucleus, and from it, on each side, they gather in a single-trunk, descending pathway, emitting branches in the cervical, thoracic and abdominal region, where they end. These preganglionic fibers will establish synapses in peripheral ganglia of the parasympathetic vegetative or autonomous nervous system, close to, or even inside, the viscera walls.
The visceral special efferent (motor) fibers of the vagus originate in the ambiguous nucleus, and are responsible for innervation of the striated muscles of the pharynx, larynx and esophagus.
The Hypoglossal (XII) nerve, a motor one, has an individualized nucleus on the ventral-medial portion on each side of the medulla oblongata. It is responsible for the tongue extrinsic and intrinsic muscles. In addition, fibers from the cervical plexus in association with the hypoglossal nerve form the ansa cervicalis, from which a branch from the cervical plexus, usually C1, will innervate the geniohyoid muscle, one of the responsible for the hyoid-laryngeal displacement.
The pharyngeal plexus (glossopharyngeal, vagus and accessory though vagus) is considered responsible for the pharyngeal reflex phase, where afferent information from the pharynx reach the brainstem, generating efferent stimuli to the pharyngeal structures involved in this phase of the swallowing process.
The pressure transfer from the oral cavity to the pharynx by distention would produce afferent stimuli that would reach the brainstem, in special the sensitive (solitary tract) nucleus. From the sensitive nucleus, through interneurons of the reticular formation, the ventral motor (ambiguous) nucleus of the brainstem generates efferent motor stimuli to the pharyngeal structures. Several structural movements initiated during the voluntary oral phase, remain in progress until the end of the pharyngeal phase, such as hyoid-laryngeal elevation, swallowing apnea and tongue posterior projection, to pharynx, started during the oral ejection, without considering the palate tension produced by the trigeminal nerve. In this way, several elements of the oral phase incorporated by the pharyngeal reflex phase allow us to consider the pharyngeal phase as dependent on the cranial nerves V, VII, IX, X, XI and XII of both sides.
To command your guts you need
- Carminatives are aromatic herbs containing volatile oils. These small molecules help relieve gas, tension and spasm. They help the digestive process function smoothly and with ease.
- Bitters are stimulating to the secretions of stomach, pancreas, liver and small intestines, and increase our ability to digest and assimilate our food.
- Demulcents are slimy, mucilaginous herbs. They are made up of branched carbohydrate molecules that easily trap water and other molecules, causing them to swell and become like soft sponges. These herbs are very soothing to the gut walls and the nerves.
- Nervines are relaxing herbs that are often tonic or supportive to the nervous system.
Bitters are used when there is indigestion, heartburn, poor fat digestion or constipation.
Demulcents are used when any of the GI tract mucous membranes are irritated, ulcerated or inflamed – from the throat on down, and for watery stools.
Carminative nervines - lemon balm, chamomile, lavender, hawthorn, rosemary, valerian, peppermint, hyssop, celery seed
Carminative bitters – turmeric, angelica, elecampane, wormwood, mugwort
Bitter nervines – motherwort, blue vervain, hops, skullcap
Demulcent nervines – linden, oats Other demulcents – marshmallow, slippery elm, plantain, flax
Beneficial Herbs for Digestion
Our DIY digestive bitters recipe uses the following beneficial herbs:
ANGELICA. Angelica is a stimulant, which aids in gastrointestinal secretions, absorption, and elimination. It relieves gas and the feeling of fullness. (Avoid if pregnant).
GENTIAN. Gentian is a simple bitter that has been used for over 3,000 years to revitalize the gastrointestinal tract by optimizing levels of stomach acid and digestive enzymes. Gentian is especially helpful for protein and fat digestion. (Avoid if pregnant or on H2 receptor antagonists, like Zantac, or other antacids).
DANDELION. Dandelion is high in nutrients and is bitter, which stimulates the cascade of digestive secretions. Dandelion also has a significant cleansing effect on the liver by stimulating bile production, which is important for fat digestion.
GINGER. Known as the “universal medicine,” ginger is warming and carminative, which means it’s great at relieving bloating and gas. Ginger also supports healthy bowel movements.










No comments:
Post a Comment