Death stalks all of us upon this planet! Nevertheless, had it not been for the confusion of the struggle I would have been circumscribed by short boundaries of my pain and suffering squealing with fright.
When I had two surgeries back to back and the doctor said, "Everything is in God's hands", and I came to unexpectedly with drainage tubes and wires hooked up onto me and were discharged from the hospital with two with drainage bags dangling on both sides I had to just switch off my mind from the physical confinement of pain, facing medical embarrassments, the humiliation of asking for financial help to pay the hospital bill for the sudden surgery because it happened during the time of demonetisation.
Physical suffering is always there with a rare disease and especially when doctors go wrong. But I was never aware of a pain that lingers long, very, very long.
I always thought comfort lay in the knowledge although it is hardly worth reading or knowing about if you feel fear softly following you along the darkening streets of life, you got to understand that information, awareness, understanding, depth of thought dispels fear, worry or stress. Sitting in the darkness I started seeking knowledge of the ways of nature. A dark gloomy world, it definitely seemed but I read whatever I could lay my hands on. I have a serious condition known as "Abibliophobia" but I am not here to explain that.
Strange but true we are afloat in a broad sea 🌊 anchor-less,
Fear sets in when we shed a tear in aloneness,
Ah! What a mess!
" Have no fear!" said Hope,
"When the Sun gets sunny,
We will have a lot of things that are very funny."
So I say never stop believing in hope because miracles can happen any moment! A lot should be shared with others from what I have learned in a simplified way, so here it goes…
The rarity of CNS leptomeningeal hemangioblastomas.
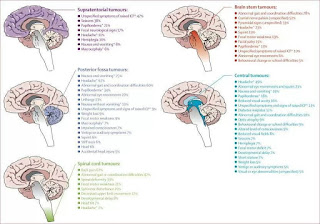
Brain tumours grow within a rigid, firm bony skull. Benign, slowly growing or malignant brain tumours may produce serious neurological symptoms and signs prior to treatment or cure. Although brain tumours rarely metastasize outside the central nervous system (CNS), disability and death occur with brain tumours when the intracranial contents exceed the intracranial space, causing herniation and compression of respiratory centres.
Fewer than 5% of patients with brain tumours have a predisposing genetic syndrome. The most common of these are von Recklinghausen's types I and II neurofibromatosis, tuberous sclerosis, von Hippel-Lindau disease, and the epidermal nevus syndrome. These dominantly inherited neurocutaneous syndromes are associated with an increased incidence of specific tumours.
There are more than 120 types of tumours of the CNS.
Neuroepithelial tumours are the most common and feared tumours of adult life and occur most frequently as astrocytoma, oligodendroglioma, and ependymoma.
Leptomeningeal hemangioblastomas are perhaps the rarest sort.
What is a hemangioblastoma?
Hemangioblastomas (HBs) of the central nervous system (CNS) are histologically benign, slow-growing tumours, which may occur as sporadic lesions or in association with von HippelLindau (VHL) disease.
What is von Hippel-Lindau or VHL?
von Hippel Lindau is a very rare disease.
von Hippel-Lindau or VHL which is a genetic defect that causes capillary growth to go out of control. While the tiniest blood vessels or capillaries usually branch out gracefully like trees, in VHL patients a little knot of extra capillaries forms a growth or tumour and in certain cases, it turns cancerous. It is a genetic form of cancer VHL patients battle a series of tumours throughout their life.
VHL may occur in up to 10 organs of the body like liver, kidney, brain, spinal cord or retina, inner ear, pancreas. There is a possibility of neuroendocrine tumours.
What are the leptomeninges?
Meninges are the three membranous envelopes—pia mater, arachnoid, and dura mater, that surround the brain and spinal cord. Cerebrospinal fluid fills the ventricles of the brain and the space between the pia mater and the arachnoid. The primary function of the meninges and of the cerebrospinal fluid is to protect the central nervous system.
The two innermost layers of tissue, arachnoid mater and pia mater that cover the brain and spinal cord are together called the leptomeninges.
Leptomeningeal dissemination of Hemangioblastomas
Hemangioblastomas of the CNS are solid or cystic vascular-rich tumours, most common in the cerebellum, less frequent in the brainstem or spinal cord and rare in supratentorial locations with meningeal involvement.
Bakshi et al3 described a 55-year-old patient with disseminated intradural masses involving almost the entire spinal cord on magnetic resonance imaging. They reported both extramedullary intradural tumour with numerous leptomeningeal nodules and microscopic infiltration of the spinal cord and coined the term leptomeningeal hemangioblastomatosis to define this condition.
Hemangioblastomas of the central nervous system are the most common tumours seen in patients with von Hippel-Lindau (VHL) disease.
Leptomeningeal dissemination of hemangioblastomas (HB) of the central nervous system (CNS) is extremely rare. Between 1902 and 2013, approximately 132 cases were reported. Few studies have reported leptomeningeal involvement in sporadic HB or in HB associated with von HippelLindau syndrome.
Diffuse infiltration of the leptomeninges is known as hemangioblastomatosis and has been observed both in VHL disease and in patients with spontaneous mutations.
Treatment
Detecting and treating the condition of leptomeningeal hemangioblastoma without delay seems to help survival, though the number of patients analysed is small. Patients may have other underlying health issues which may affect the data.
Because no case of de novo development of disseminated HB without previous surgery has been reported, it is strongly suggested that the spillage and spread of tumour cells through the CSF space may be an origin of hemangioblastomatosis in patients with a genetic predisposition to the condition, Care should be taken to avoid tumour cell spillage during surgery.
Prior to surgery of the initial tumour, planned embolization should be undertaken if possible to reduce blood loss. However, depending on the actual tumour structure embolization may be found not to be possible. Reducing blood loss may also help in reducing tumour cell spillage and spread.
Looking at tumour cells in the spinal fluid under high-resolution MRI scans are all that is necessary for an accurate diagnosis. A biopsy isn't required for diagnosis as it may cause meningitis and blood loss thereby cell spillage.
My experience with leptomeningeal hemangioblastomas for 7 years?
I was diagnosed with supranational leptomeningeal hemangioblastomas in 2013. I have been seeking anyone experiencing the same condition but didn't find anyone till now.
A fellow remarked after he saw the picture of the scan of my brain tumours
" you have more tumours in the brain than people have lice in hair.''
There is no data on the competence of the surgeons and equipment used in the initial CNS surgery so trying to determine if cell spread was caused by any incompetence during my brain surgery (craniotomy) in 2006 would be extremely difficult if not impossible to prove beyond a reasonable doubt. The fact that the physiology of each tumour is different and the number of cases is so small means that an accurate comparison of surgeons is impossible.
I get stereotactic radio-surgery before the growing tumours start putting pressure on the brain and become symptomatic. I have lost vision of my right eye for not being able to avail radiation therapy at the right time because of financial reasons and also because I was diagnosed with an RCC ( kidney cancer) at the same time.
Advanced radiation techniques, such as radiosurgery, are more effective than conventionally fractionated radiotherapy, but it is difficult to perform high-dose radiation therapy or radiosurgery for numerous lesions scattered throughout the brain.
Radiosurgery appears to be safe and has prevented local recurrences in my case, with fewer sessions than conventional radiation which caused white matter changes representing chronic ischemic changes. I couldn't afford a cyberknife and underwent conventional radiation therapy in 2017 after which this happened.
Sometimes tumours treated with radiation, on follow-up MRI imaging scans, appear stable without evidence of growth even mildly shrinking every time.
Unexplored safe technology.
It is a new exciting technology which may help people trying to minimise collateral damage which with radiation treatments has always been the challenge.
The precision of proton therapy can be critical for protecting the brain’s delicate tissues.
Proton therapy can limit the amount of normal brain tissue receiving radiation. That reduces the effects on important functions, such as vision and hearing.
Proton radiation may be less likely to damage nearby organs, such as the heart and lungs while treating areas around the spinal cord. This technique is safe and potentially effective.
Often, people with these recurrent tumours have received significant radiation doses in the past to important parts of the brain. These may include optic nerves, which are critical to vision, and the brainstem, which regulates many essential body functions, such as breathing, heart rate, and swallowing.
To treat more people with proton therapy is by making the technology even more accessible. Currently, this technology is available only in Apollo Chennai and expensive enough to cost an arm and leg.
If only, governments or some trust or Institute sponsors the high cost of my treatment. I could have a better and longer life and my quality of life would be better.
References
Hemangioblastomas with leptomeningeal dissemination: case series and review of the literature in journal Acta Neurochirurgica.
Supratentorial leptomeningeal hemangioblastoma resection after preoperative embolization Lee, Ching-Yi, Chen, Shiu-JauLanguage: English Journal: Formosan Journal of Surgery.
Journal of Korean Medical Science, article Arch Pathol Lab Med--Vol 132, January 2008- Intradural Extramedullary Leptomeningeal Hemangioblastomatosis and Paraneoplastic Limbic Encephalitis Diagnosed at Autopsy
Journal Neuropathology -A report of supratentorial leptomeningeal hemangioblastoma and a literature review
Power and Precision: Proton Therapy Can Target Brain and Spine Tumors with Fewer Side Effects
I might add a finishing touch,
" When you hear good eats think of horses not zebras" …
This is told to medical students throughout their training.
In medicine, the term "zebra" is used in reference to a rare disease or condition. Physicians are taught to assume that the simplest explanation is usually the best so as not to go around diagnosing patients with all sorts of unfamiliar illnesses that are highly unlikely. Common diseases are what doctors should expect to encounter.
Many medics seem to forget" zebras 🦓" exist and so getting diagnosis and treatment is difficult for those who have a rare disease.
While spending hours in front of the silvered mirror admiring the scars of a liver transplant, partial nephrectomy, incisional hernia repair which led to the unfortunate debridement, when I asked the brightest medical mind
" Am I going to die?"
His rejoinder was
"We cannot let that happen, you are our precious patient." but the surgeon who was supposed to do the debridement said
" Everything is in God's hands"... I nodded and the very next morning they made arrangements for my admission and surgery. While I was hooked onto machines, punctured with needles and tubes going through them inside the operation theatre I was made to sit up and sign some sort of register. When the surgery was a success I showed an upturned thumb to the doctor because God helped him see the right path.
So, all I see while looking at myself in the mirror, what I find is a strong, wild, badass Unicorn 🦄.
Mermaids and unicorns are among the world's best-known mythical creatures but bats🦇 aren't. So, why such a delay in tracing the origin of the virus which spread and triggered a global pandemic creating a historical health crisis and a deeply distressing and disturbing experience for many?


Payel has thoroughly researched her condition of "leptomeningeal hemangioblastomas". The possible cause and treatments are given. There are few patients who are able to describe their own illness using such scientific terminology that would be suitable for entering into a doctorate thesis. The difficulty of getting funding for expensive treatment in India is also described. Treating ultra-rare conditions successfully benefits everyone as it increases medical knowlwdge that is applicable to all.
ReplyDeleteThroughout this Payel's determination to win through shines - the true warrior that she is.